Innovation & Transformation
The South Carolina Oral Health Action Network (SCOHAN) is a dynamic and forward-thinking organization dedicated to revolutionizing oral health in South Carolina. Comprising oral health stakeholders, public and private entities, and community-based organizations, SCOHAN is committed to finding innovative solutions that support, promote, and enhance oral health for every individual across the state. As a responsive initiative aligned with Priority 1 of the South Carolina State Oral Health Plan, SCOHAN aims to address lifespan oral health challenges and issues affecting our population.
Oral health innovation and transformation in South Carolina involves collaborative efforts, evidence-based initiatives, and preventive strategies to improve the oral health status of all South Carolinians. Organizations like the BlueCross BlueShield of South Carolina Foundation foster a culture of quality improvement and innovation in the oral health care system. SCOHAN finds it imperative to investigate new and novel ideas around early oral cancer detection, community water fluoridation, and rural oral heath initiatives. South Carolina’s oral health transformation involves strategic planning, collaboration, and a commitment to evidence-based practices. By addressing disparities and promoting preventive measures, the state aims to enhance the well-being of its residents through better oral health.
The recently launched 2022-2026 South Carolina State Oral Health Plan (SOHP), serves as our roadmap. Developed through extensive collaboration and data-driven insights, this plan outlines our collective efforts to elevate oral health across the state.
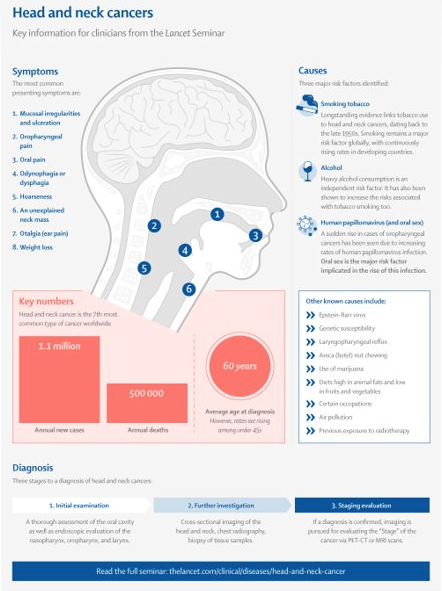
Head and neck cancers are a deadly cancer that ranks among the six most common cancers worldwide. (American Cancer Society, 2021). Studies have shown a greater disease burden among minority populations for head and neck cancer, higher mortality rates, and lower oral cancer knowledge, but limited evidence has defined the underlying causes of late-stage diagnoses and access to the healthcare system (Suzuki et al, 2019).
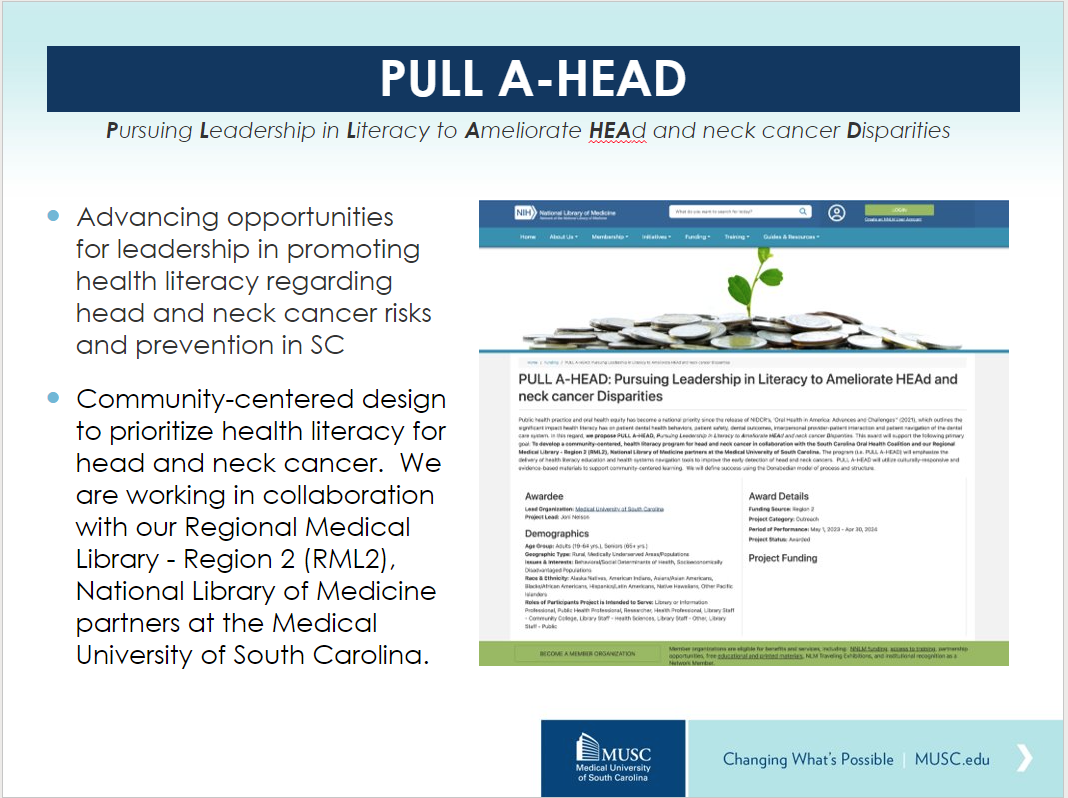
PULL AHEAD aims to develop and implement a community-centered approach design for increasing the health literacy and efficacy of navigating the healthcare system for early detection of head and neck cancers. The program (i.e. PULL A-HEAD) will emphasize the delivery of health literacy education and health systems navigation tools to improve the early detection of head and neck cancers.
- In comparison to the national rates, South Carolina is among the top ten for head and neck cancers (Community Outreach, Hollings Cancer Center, MUSC, 2019).
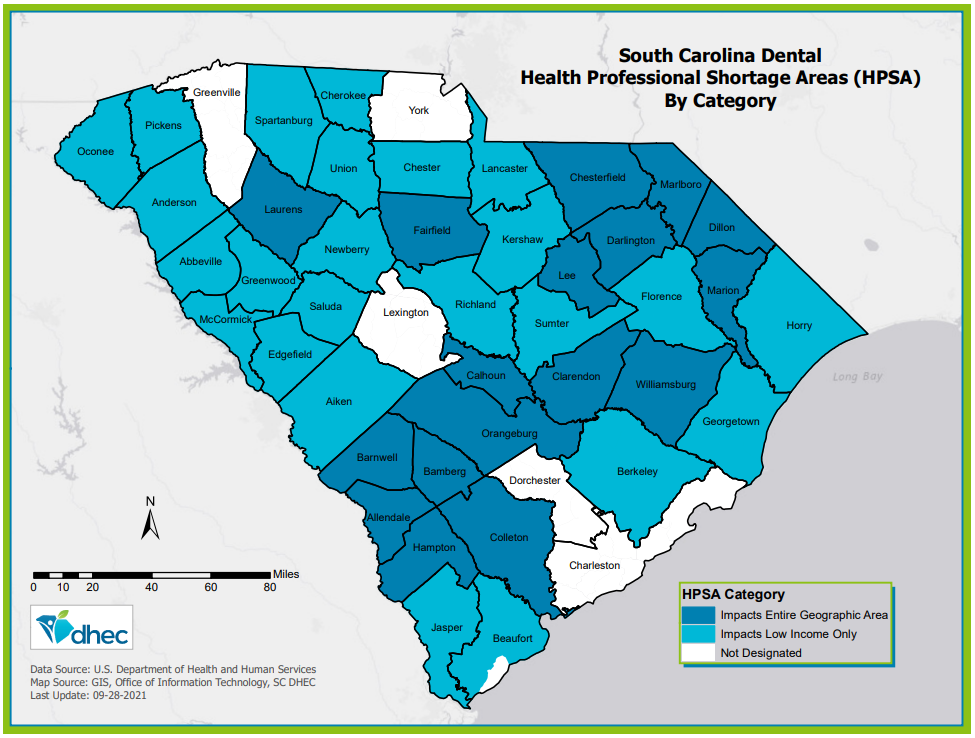
- SC currently has 44 of 46 counties designated as geographic Primary Care and Dental Health Professional Shortage Areas and approximately 25% of SC citizenry are living in rural areas (HRSA, 2018).
- Rural communities face unique challenges to achieving optimal oral health, impacted mainly by geographic location and socioeconomic status (IOM&NRC, 2011). More specifically, rural southern states such as SC continue to have a tremendous shortage of primary care providers.
- Dental and primary care play a critical role in delivering quality patient education, prevention, risk reduction, and treatment regimes.
To enhance the quality and equity of oral cancer prevention in rural SC, we must prioritize strategies to elevate the significance of head and neck cancer risks. Therefore, the need to design and deliver innovative strategies to increase opportunities that intersect the healthcare system and community is inevitable.
Joni D. Nelson, Irene M. Lubker. Pursuing leadership in literacy to ameliorate head and neck cancer disparities [abstract]. In: Proceedings of the American Association for Cancer Research Annual Meeting 2024; Part 1 (Regular Abstracts); 2024 Apr 5-10; San Diego, CA. Philadelphia (PA): AACR; Cancer Res 2024;84(6_Suppl):Abstract nr 998
PULL A-HEAD: Pursuing Leadership in Literacy to Ameliorate HEAd and neck cancer Disparities
- Head and neck squamous cell carcinoma (HNSCC) accounts for roughly 4.5% of cancer diagnoses and deaths (Barsouk et al. 2023)
- In a study of racial disparities among surgically treated head and neck (HNC) patients, black patients’ mortality was 19% higher than white patients (Jassal et al, 2021)
- HPV accounts for 72% of all head and neck squamous cell carcinoma cases in developed nations (De Martel et al, 2012)
- South Carolina is among the top ten for head and neck cancers (MUSC Hollings Cancer Center, 2019)
What Have We Done
- In alignment with NNLM’s framework to improve the public’s health through enhancing an individuals’ access to information for future informed decisions about their health, in this we aim to:
- Goal 1. To develop a community-centered, health literacy program to prioritize head and neck cancer screening and prevention
- Objective a. Conduct a formative exploration of head and neck cancer knowledge, resources, and health navigation tools in rural and underserved communities of SC;
- Objective b. Develop culturally responsive and evidence-based materials for the PULL A-HEAD health literacy and health navigation toolkit for community stakeholders and clinical providers;
- Goal 2. To establish a health advocacy network for head and neck cancer among RML R2 partners
- Objective c. Collaborate with the RML R2 Organization, SC Libraries and allied personnel, SC Oral Health Action Network, MUSC Health Literacy Think Tank, and MUSC to guide stakeholder engagement regarding the development of PULL A-HEAD and related advocacy efforts in South Carolina
Preliminary Findings
- Public librarians agree that they have more knowledge of their communities and how to provide the education
- Public librarians prefer opportunities to partner with local dentists to advance health literacy among their community residents
- Education and health literacy on head and neck cancer are not currently being prioritized in libraries
- Public libraries receive good attendance at health-related library programs
- Public library reference resources could be enhanced by the inclusion of head and neck cancer-specific information
Cancer Prevention
More than one-third of all cancer patients develop complications that affect the mouth, according to the National Institute of Dental and Craniofacial Research. These mild to severe side effects can include mouth sores, infection, dry mouth, sensitive gums, and jaw pain.
Your mouth health is an important part of your overall health, so make your dentist part of your cancer care team.
Oral Cancer Resources
- Collaboration to Prevent Head and Neck Cancers
- National Institutes of Health: Chemotherapy and Your Mouth (pdf)
- Detecting Oral Cancer: A Guide for Healthcare Professionals(pdf)
- South Carolina Cancer Alliance
- South Carolina State Cancer Plan
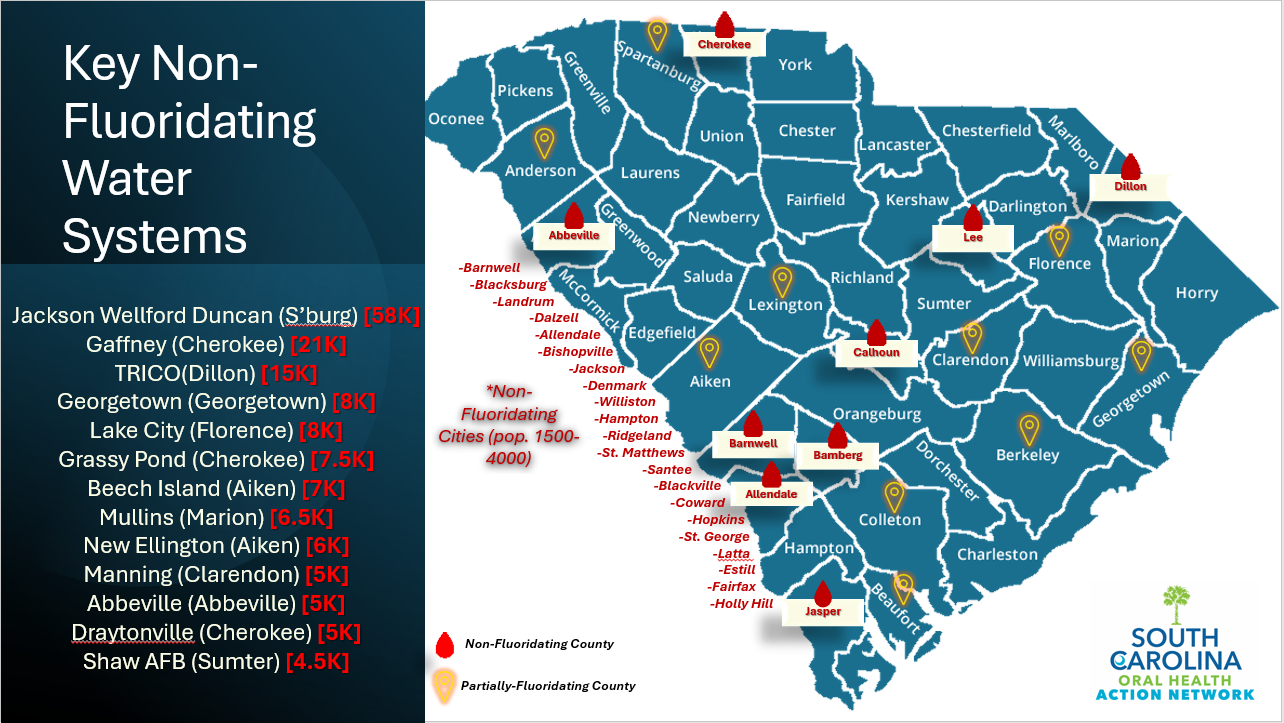
Community Water Fluoridation
Community leaders have come to realize that fluoridation benefits their entire community—children, adults, and age groups 65 and up. Community water fluoridation does not discriminate against anyone based on income, education, or race. Simply by drinking fluoridated water, everyone in a community benefits. Even today, with other available sources of fluoride, studies show that water fluoridation reduces tooth decay by about 25 percent over a person’s lifetime.
Because of the important role community water fluoridation has played in the reduction of tooth decay, the Centers for Disease Control and Prevention (CDC) has proclaimed community water fluoridation one of 10 great public health achievements of the 20th century.
Current Statistics
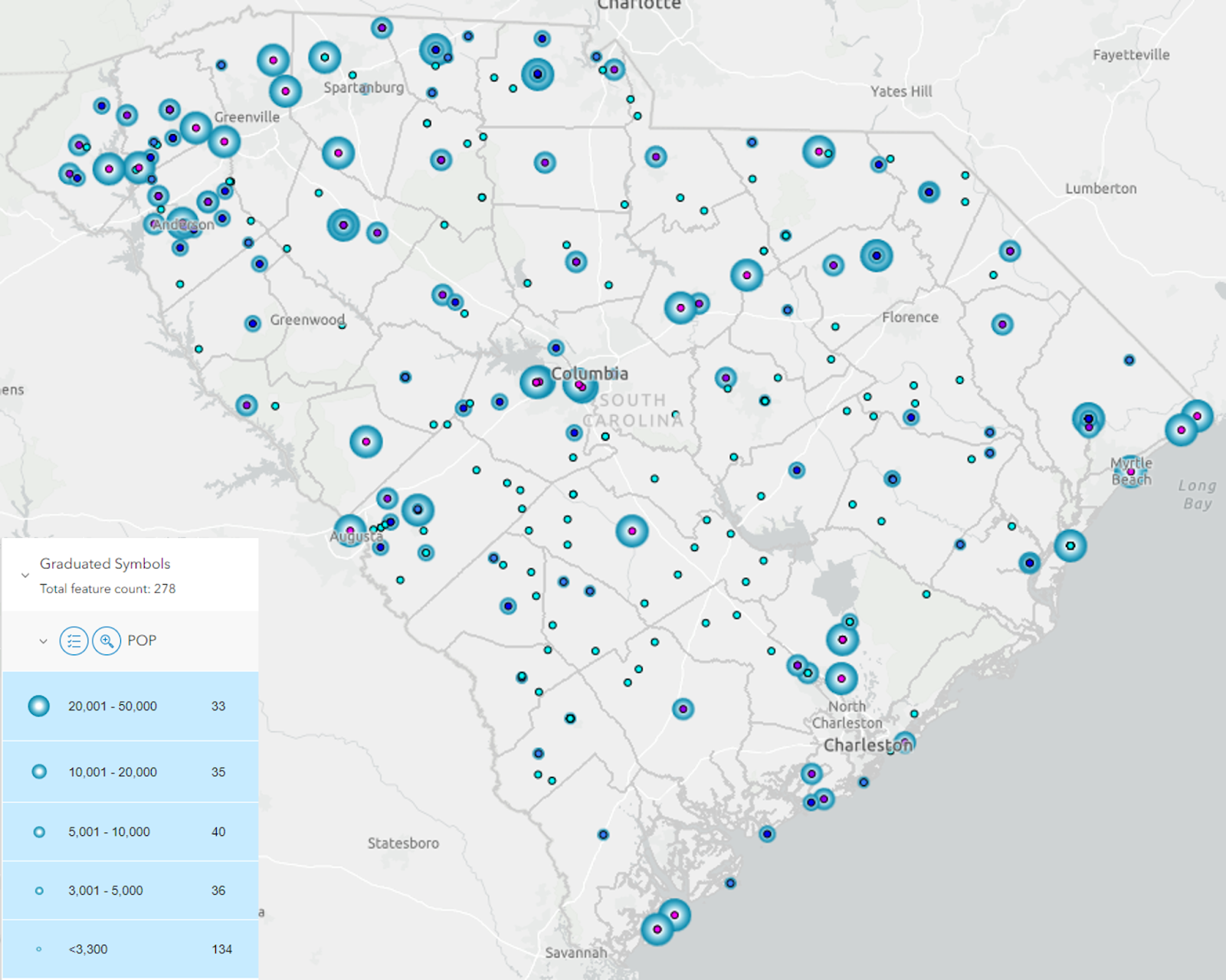
Currently, South Carolina has 41 community water systems that adjust Fluoride levels. Many of the water operators have begun treating the recommendation as an EPA listed Maximum Contaminant Level (MCL), thereby maintaining a fluoride level below the recommendation. Today, approximately 15 (36.6%) of these systems are adjusting fluoride levels at 0.70 mg/L or lower. Only 26 systems (63.4%) are adjusting fluoride levels in compliance with the 2015 CDC and DHHS recommendation. 38 water systems provide water with natural fluoride levels. Since the release of the 2015 recommendation, SC tracking data indicate that the percentage of people on community water systems with access to fluoridated water has increased to 92% and those with access to water that meets the 2015 recommended level (0.70-1.2 mg/L) is only 30.03%.
South Carolina Water Fluoridation Map
Does My County Fluoridate?
South Carolina Community Water Systems by Population
Water Systems serving 10,000 or less
South Carolina Community Water Fluoridation Fact Sheet (pdf)
Community water fluoridation continues to be the most cost-effective, equitable, and safe means to protect from tooth decay in our community. For more information and resources on fluoridation, visit https://scDPH.gov/health/oral-health/child-and-teen-oral-health/fluoridation
Additional Fluoridation Resources
South Carolina Community Water Fluoridation Plan (pdf)
South Carolina Rural Water Association
The South Carolina Rural Water Association was established in 1976. SCRWA is a non-profit trade association that assists public and private water/wastewater systems state-wide to ensure that the residents of South Carolina have access to clean water. We help deliver Quality on Tap!
CDC Water Fluoridation Course
Utilize this free resource designed by the CDC to build the capability of state fluoridation programs and to help increase knowledge and refine skills to implement and maintain community water fluoridation.
Oral Health in Rural Communities
The regular preventive care of the teeth and gums is important in maintaining quality of life and overall health, playing a role in controlling diseases such as diabetes and heart disease. Yet, rural communities often lack adequate oral healthcare and subsequently miss out on the benefits of good oral health as well. Several factors have been well documented as contributing to the oral health challenges of rural America:
- Access to dental care – Many rural communities lack access to oral health providers due to geographic isolation and workforce maldistribution.
- Oral health literacy – A 2009 study found that health literacy is lower among rural populations. In terms of oral health, poor health literacy can result in poor oral hygiene and difficulty in navigating the oral health system. In addition, rural residents with low health literacy are more likely to consume sugar-sweetened beverages and more prone to dental caries, according to a 2016 report.
- Fluoridation of water supplies – A higher proportion of homes in rural communities are not served by community water systems and as a result cannot receive the preventive benefits of optimally fluoridated water.
- Tobacco use – Cigarette smoking is more prevalent in rural areas than in urban areas (26.7% of adults in nonmetro areas vs. 16.2% of adults in large metro areas), as well as smokeless tobacco use (6.2% of adults in nonmetro areas vs. 2.0% of adults in large metro areas), according to a 2022 SAMHSA report.
Additional Rural Oral Health Resources
- Evidence-Based Toolkits for Rural Community Health
- Promising Practices for Increasing Access to Transportation in Rural Communities
- Senate Hearing on the Dental Crisis in America, Health Education Labor & Pensions
- CPSTF Findings for Oral Health
- The Community Guide: Oral Health
- Rural Oral Health Toolkit
- Healthy People 2030
- Updates from the SCPHCA